Diabetic Kidney Disease
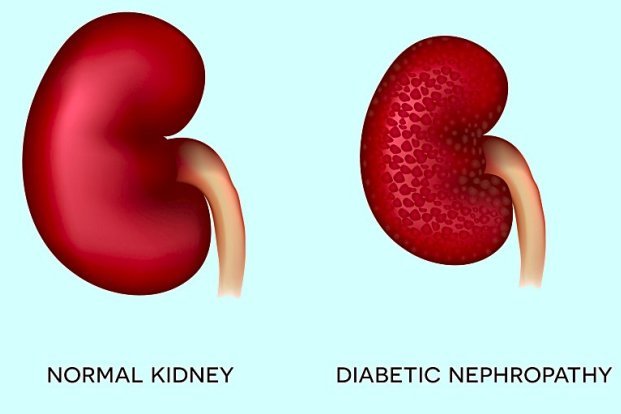
What is Diabetic Kidney Disease?
Symptoms of Diabetic Kidney Disease
In the early stages, DKD often shows no symptoms. As the disease progresses, common symptoms include:
Swelling in feet, ankles, hands, or eyes (due to fluid retention)
Increased need to urinate, especially at night
Reduced need for insulin or diabetes medicines (as kidneys fail to break down insulin)
High blood pressure (hypertension)
Fatigue and weakness
Nausea or vomiting
Loss of appetite
Persistent itching
Shortness of breath (due to fluid accumulation in lungs)
Confusion or difficulty concentrating
Procedure or Treatment for Diabetic Kidney Disease
Treatment for diabetic kidney disease focuses on slowing disease progression and managing symptoms. This includes:
Blood Sugar Control – Maintaining target blood glucose levels through medications, insulin therapy, and lifestyle changes.
Blood Pressure Control – Using ACE inhibitors or ARBs to protect kidneys even if blood pressure is normal.
Dietary Modifications – Limiting salt, protein, and potassium intake to reduce kidney load.
Medications – Including sodium-glucose co-transporter-2 (SGLT2) inhibitors that provide renal protection.
Regular Monitoring – Periodic urine and blood tests to assess kidney function and protein leakage.
Dialysis – In advanced stages when kidneys fail to function effectively.
Kidney Transplant – For patients with end-stage renal disease to replace the failed kidney.
Prevention of Diabetic Kidney Disease
Preventing DKD involves strict management of diabetes and other associated risk factors:
Maintain optimal blood sugar levels
Control blood pressure within target range
Adopt a kidney-friendly diet with low salt and protein
Exercise regularly to maintain healthy weight
Avoid smoking and limit alcohol intake
Stay hydrated
Regularly monitor kidney function and urine protein levels
Follow prescribed medications without skipping doses
Benefits of Early Detection and Treatment
- Slows down kidney damage progression
- Reduces risk of developing end-stage renal disease
- Prevents complications such as heart disease and stroke
- Improves quality of life and overall health
- Minimises need for dialysis or transplant in later life
Types of Diabetic Kidney Disease
Though broadly categorised as diabetic nephropathy, it can be classified based on stages:
Stage 1 (Hyperfiltration) – Increased kidney filtration without symptoms.
Stage 2 (Silent Stage) – Minor structural changes with normal kidney function.
Stage 3 (Microalbuminuria) – Small amounts of protein leak into urine.
Stage 4 (Macroalbuminuria) – Large amounts of protein leak; kidney function declines.
Stage 5 (End-Stage Renal Disease) – Severe kidney failure requiring dialysis or transplant.
Why Choose for Diabetic Kidney Disease?
Our experienced nephrologists and diabetologists provide comprehensive care for diabetic kidney disease. We focus on early detection, personalised treatment plans, and continuous monitoring to prevent complications and improve patient outcomes. Our advanced dialysis unit and kidney transplant consultation services ensure complete renal care under one roof.
