Reno Vascular Hypertension
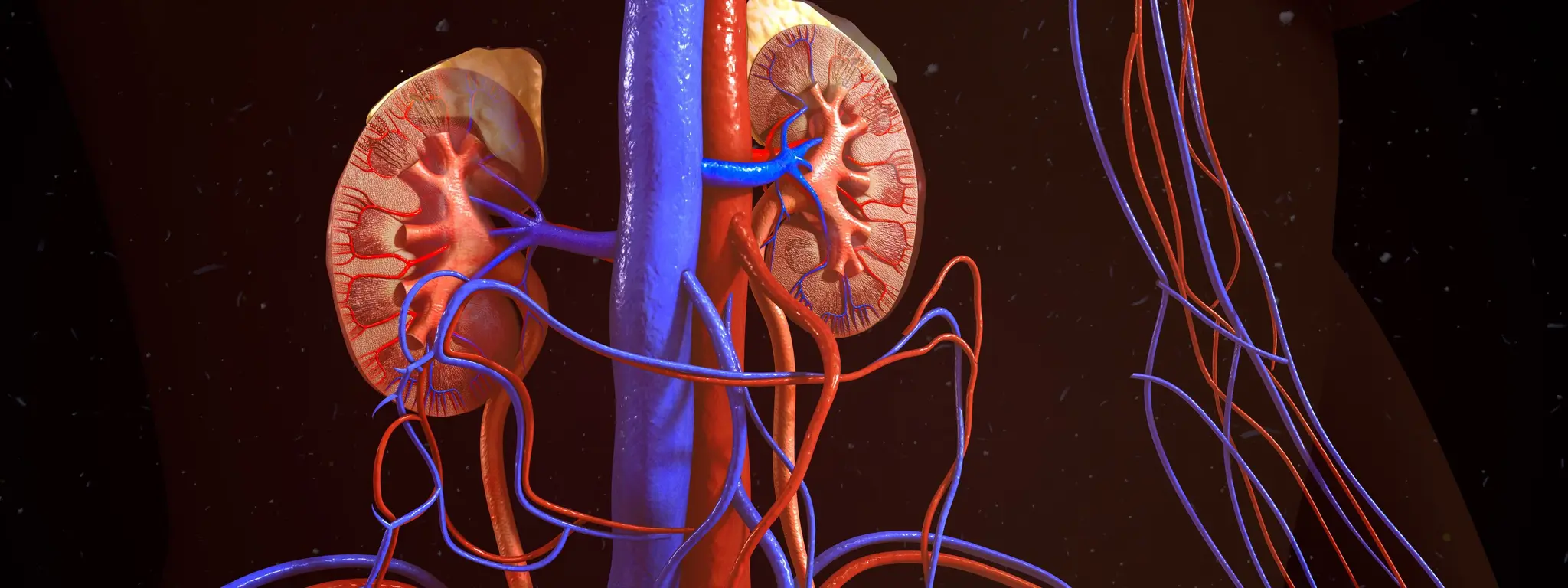
Reno Vascular Hypertension
Causes of Reno Vascular Hypertension
Atherosclerosis:
Most common cause, especially in older adults.
Fatty plaque builds up in the renal arteries, narrowing the vessel and reducing blood flow to the kidneys.
Fibromuscular Dysplasia (FMD):
More common in younger individuals, particularly women.
Abnormal growth or thickening of the artery walls causes narrowing or twisting of the renal arteries.
Renal Artery Thrombosis or Embolism:
Blood clot blocks the renal artery suddenly, leading to a drop in kidney blood flow and a rise in blood pressure.
Renal Artery Aneurysm:
Bulging or weakening in the artery wall can affect blood flow and contribute to hypertension.
Vasculitis:
Inflammation of blood vessels, including renal arteries, can reduce blood supply to the kidneys.
External Compression:
Tumors or other masses near the kidneys may compress renal arteries and limit blood flow.
Congenital Abnormalities:
Rare structural abnormalities of the renal arteries present from birth can also cause narrowing.
Each of these conditions reduces blood flow to the kidneys, which triggers hormonal responses that increase blood pressure.
Symptoms of Renovascular Hypertension
Renovascular hypertension often has no obvious symptoms in its early stages. However, as the condition progresses, you may notice:
Severe or resistant high blood pressure
– Blood pressure that is hard to control with standard medications.Sudden onset of high blood pressure
– Especially in people under 30 or over 55 years old.Worsening kidney function
– Increased creatinine levels, especially after starting blood pressure medications like ACE inhibitors or ARBs.Abdominal bruit
– A whooshing sound heard with a stethoscope over the abdomen (caused by turbulent blood flow in narrowed renal arteries).Swelling in the legs or ankles
– Due to fluid retention if kidney function is impaired.Frequent headaches
– Related to uncontrolled blood pressure.Blurred vision or dizziness
– Signs of high blood pressure affecting other organs.Fatigue or weakness
– Due to reduced kidney function or high blood pressure effects.
Procedural Treatments for Renovascular Hypertension
1. Percutaneous Transluminal Renal Angioplasty (PTRA):
What it is: A minimally invasive procedure to open narrowed renal arteries.
How it works:
A thin catheter with a balloon at its tip is inserted into a blood vessel (usually in the groin).
The catheter is guided to the narrowed renal artery.
The balloon is inflated to widen the artery and improve blood flow.
When it’s used: Common in fibromuscular dysplasia or in patients who can’t tolerate medications.
2. Renal Artery Stenting:
What it is: Often done along with angioplasty.
How it works:
After the balloon widens the artery, a small mesh tube (stent) is placed to keep the artery open.
When it’s used: Particularly useful in atherosclerotic renal artery stenosis, especially if there is significant blockage.
3. Surgical Revascularization (Renal Artery Bypass Surgery):
What it is: An open surgery where a healthy blood vessel (usually from another part of the body) is used to bypass the blocked renal artery.
When it’s used: Reserved for complex cases where angioplasty and stenting are not suitable (e.g., multiple blockages, aneurysms, failed prior procedures).
4. Nephrectomy (Rarely Used):
What it is: Surgical removal of one kidney.
When it’s used: In rare cases where one kidney is non-functioning and causing uncontrolled hypertension, removal may help control BP.
