Acute Renal Failure
Acute Renal Failure
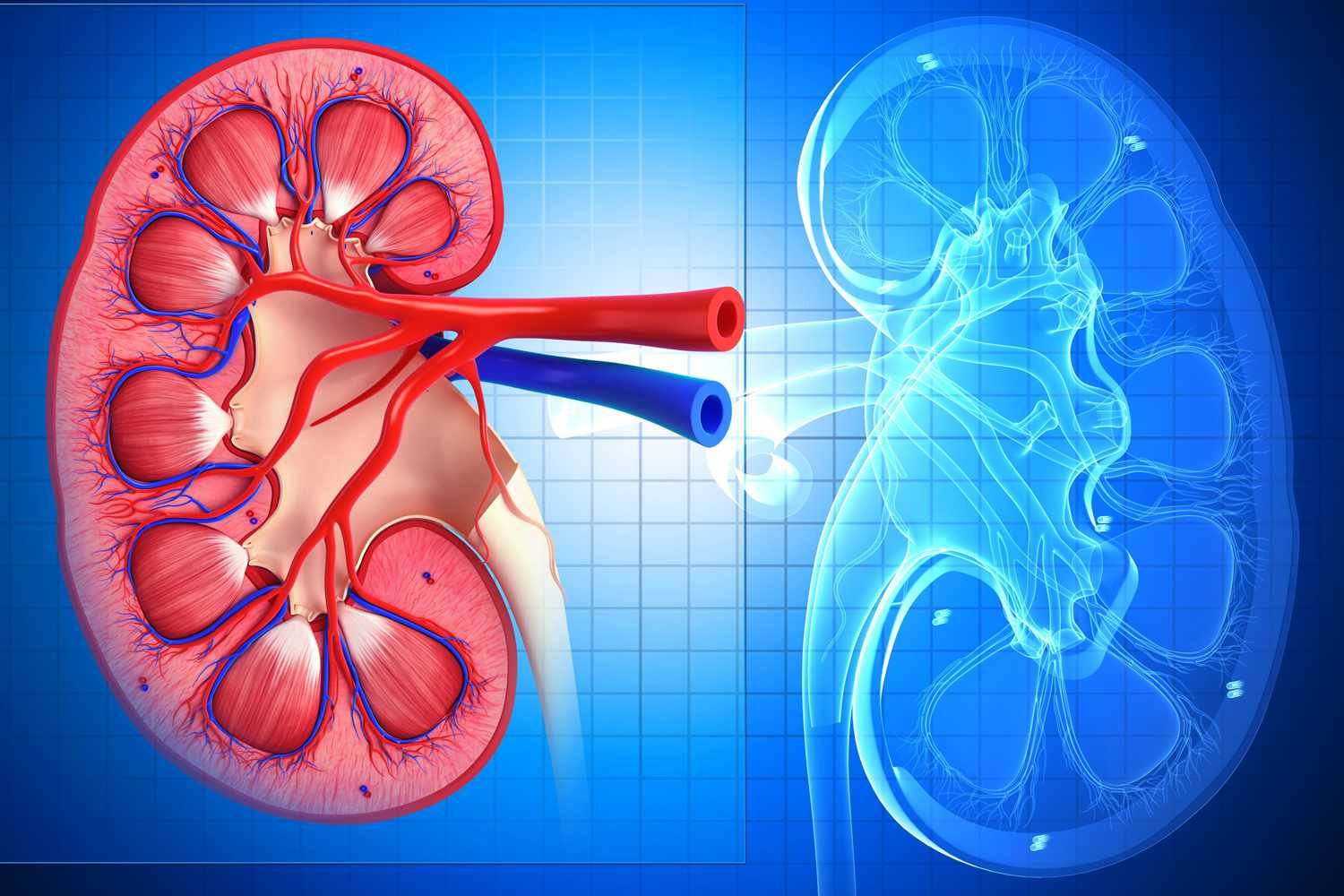
Acute Renal Failure (ARF), also known as Acute Kidney Injury (AKI), is a sudden loss of kidney function over hours to days. It leads to the accumulation of waste products, electrolyte imbalances, and fluid overload. Unlike chronic kidney disease (CKD), ARF is often reversible if diagnosed and treated promptly.
Causes of Acute Renal Failure
A. Pre-Renal (Reduced Blood Flow to Kidneys)
- Hypovolemia (severe dehydration, hemorrhage, burns)
- Cardiogenic shock (heart failure, myocardial infarction)
- Renal artery stenosis or thrombosis
- Severe hypotension (sepsis, anaphylaxis)
B. Intrinsic Renal (Direct Kidney Damage)
- Acute tubular necrosis (ATN) – Most common cause (ischemia, toxins like NSAIDs, contrast dye, antibiotics)
- Glomerulonephritis (post-streptococcal, lupus nephritis)
- Interstitial nephritis (drug-induced: penicillin, diuretics, NSAIDs)
- Vascular disorders (vasculitis, thrombotic microangiopathy)
C. Post-Renal (Urinary Tract Obstruction)
- Kidney stones (bilateral ureteral obstruction)
- Bladder outlet obstruction (BPH, prostate cancer)
- Tumors (cervical cancer, colon cancer compressing ureters)
- Neurogenic bladder (spinal cord injury)
Symptoms of Acute Renal Failure
- Oliguria (reduced urine output) or anuria (no urine output)
- Fluid overload (edema, pulmonary edema, hypertension)
- Fatigue, confusion, seizures (due to uremia)
- Nausea, vomiting, loss of appetite
- Electrolyte imbalances (hyperkalemia, hyponatremia, metabolic acidosis)
Diagnosis
A. Lab Tests
- Serum creatinine (↑ levels indicate kidney dysfunction)
- Blood urea nitrogen (BUN) (↑ due to impaired filtration)
- Electrolytes (hyperkalemia, hyponatremia, metabolic acidosis)
- Urinalysis (proteinuria, hematuria, casts)
B. Imaging
- Renal ultrasound (checks for obstruction, kidney size)
- CT scan/MRI (if tumor or vascular cause is suspected)
Treatment & Management
A. Pre-Renal ARF
- IV fluids (normal saline, lactated Ringer’s)
- Treat underlying cause (blood transfusion for hemorrhage, inotropes for heart failure)
B. Intrinsic Renal ARF
- Discontinue nephrotoxic drugs (NSAIDs, aminoglycosides)
- Manage electrolyte imbalances (calcium gluconate for hyperkalemia, sodium bicarbonate for acidosis)
- Dialysis (if severe uremia, hyperkalemia, or fluid overload)
C. Post-Renal ARF
- Relieve obstruction (Foley catheter for bladder obstruction, nephrostomy for ureteral blockage)
- Surgical intervention (stent placement, lithotripsy for stones)
Complications
- Chronic kidney disease (CKD)
- Cardiac arrhythmias (due to hyperkalemia)
- Pulmonary edema (fluid overload)
- Uremic encephalopathy (confusion, seizures, coma)
Prevention
- Hydration (especially before contrast imaging)
- Avoid nephrotoxic drugs (NSAIDs, aminoglycosides)
- Monitor high-risk patients (diabetes, hypertension, sepsis)
Prognosis
- Reversible if treated early (pre-renal and post-renal causes)
- Higher mortality if multi-organ failure or sepsis is present
